Sialendoscopy-Salivary Gland Endoscopy

Sialendoscopy – Salivary Gland Endoscopy – Dr Atilla Şengör
Sialendoscopy means ‘endoscopy of the salivary gland’. We perform this diagnostic procedure in patients with frequently swollen salivary glands. This is how we look inside the salivary ducts to find the cause of the blockage. As in many other specialities, we also use an endoscope here. This allows us to evaluate the large salivary glands under the chin (submandibular) and in the cheek (parotid glands). Various diseases can occur in the ducts of these glands. Salivary gland stones, duct stenosis (stenosis) and secretion condensation (mucus plugs) are the most common ones. Foreign bodies, duct polyps (flesh formations) and inflammatory diseases may also be present. When these obstruct the duct, the salivary gland swells; swelling may recur. Sialendoscopy allows us to identify the obstructive disease directly.
We do not use this method for salivary gland tumours or small salivary glands. These are not related to the duct system. The endoscopes used for salivary gland endoscopy are much thinner than other standard endoscopes. These endoscopes have three channels (grooves); optical channel, irrigation and working channel. The outer diameters of the sialendoscopes used by Dr Atilla Şengör are 1.1 mm and 1.6 mm. They are almost toothpick thin instruments. Their working grooves are 0.4 or 0.8 mm. The necessary treatment for a stone or stenosis is performed through these grooves with very thin instruments. Since we do not have advanced technology in optics, we buy sialendoscopes from abroad. The tools we use inside are the same way… For this reason, the costs in sialendoscopy are high.
Sialendoscopy is actually a short-term examination that we prefer to perform under sterile conditions. We prefer the operating theatre environment for this. We can perform sialendoscopy under local anaesthesia. However, if we encounter a stone, for example, it is better to anaesthetise the patient. Because it may take a long time to remove the stone; we prefer general anaesthesia so that the patient does not feel distressed. Interventions such as stone removal, crushing, stenosis widening and stenting can be performed during sialendoscopy. We call these stages ‘interventional sialendoscopy’.
Sialendoscopic diagnosis and treatment started to be applied in the world in the 1990s. Dr Atilla Şengör started to work on this subject in 2004. He is the pioneer of this method in our country. He developed the method of breaking in the canal (pneumatic lithotripsy). He has written local and foreign articles and still gives speeches at conferences. In 2008, he is one of the authors of the first Turkish book on this subject. You can see some of his works in the ‘Selected Publications’ section. You can see the conferences he attended/spoke at in his biography. With the era of sialendoscopy, the approach to diagnosis and treatment of salivary gland duct diseases has changed. Especially open surgeries for salivary gland stones have decreased worldwide.
Is sialendoscopy an operation?
Sialendoscopy is actually an examination method. We use it to see inside the ducts of the salivary glands. Today, we use an endoscope to see many areas of the body by illuminating and magnifying them. We can also record images in this way. The endoscopes we use in the salivary gland ducts are called ‘sialendoscopes’. The instruments used in sialendoscopy are very thin and sensitive. Sometimes the assistance of an assistant and anaesthesia may be required. Therefore, we prefer to perform sialendoscopy under operating theatre conditions.
We can call the interventions performed during sialendoscopy surgery. But these are minimal operations. We perform applications such as salivary gland stone removal or stenosis widening by working inside the duct. We only intervene in the obstructive problem, we do not remove the salivary gland. Therefore, conditions such as scarring, facial paralysis and vascular damage that can be encountered in open surgeries are not present in sialendoscopy.
What is Salivary Gland?
Salivary glands are organs that produce saliva. Saliva secretion ensures that our mouth is moist and the bites are lubricated. The role of this secretion in swallowing and digesting food is very important. The large salivary glands are called ‘major salivary glands’. They have a duct system. The major salivary glands are located on the cheek (parotid gland), under the chin (submandibular gland) and under the tongue (sublingual gland). The saliva produced by these large glands flows into the mouth through the main duct. The opening of this duct is located under the tongue or on the inside of the cheek. Today, we can access these salivary ducts by sialendoscopy. If there is a disease blocking the duct, we can diagnose and treat it.
There are also hundreds of small salivary glands in the mouth. We call these ‘minor salivary glands’. When you touch your tongue to the inside of the lips, these are the swellings that you feel rough. However, sialendoscopy cannot be performed on them because they are too small. If necessary, we remove a few of them for pathological examination.
What are the Salivary Gland Ducts?
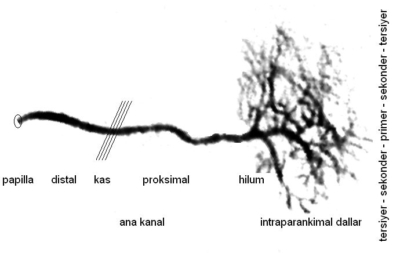
Anatomical segmentation of the salivary duct system in the sialendoscopy clinic
The salivary gland and ducts can be compared to a tree. We can think of the leafy part as the part where saliva is produced (parenchyma). Thin ducts originating from the parenchyma continue to thicken towards the trunk, just like the branches of a tree. The ducts coming from different parts of the gland merge to form the main duct (trunk). The diameter of the branches/ducts in this system varies between 0.5mm and 3.2 mm. The main duct carries saliva towards the mouth and drains it through the points we call orifices. The orifices, which are as thin as the tip of a needle, are located in the papillae. These are the bumps on the inside of the cheeks and under the tongue. Even very small stones can be caught in these funnel-shaped areas. When saliva is blocked, the gland swells. During sialendoscopy, we first enlarge this orphis and then enter the duct. We proceed in the canal system as far as the diameter of the canal allows. This distance varies between 5 and 9 cm.
As I mentioned above, the duct system is like a tree; the branches continue into the gland. Therefore, there is no such distinction as ‘inside the gland’ or ‘in the duct’ for a stone in endoscopy. These expressions are often used erroneously by those who do not perform sialendoscopy or have poor knowledge of anatomy. When we enter the duct with a sialendoscope, we can reach 80-85% of the stones regardless of the duct-gland distinction. Anyway, stones are usually in the main duct or thick branches. Problems in the thin and end branches do not cause swelling of the entire gland and do not cause significant complaints.
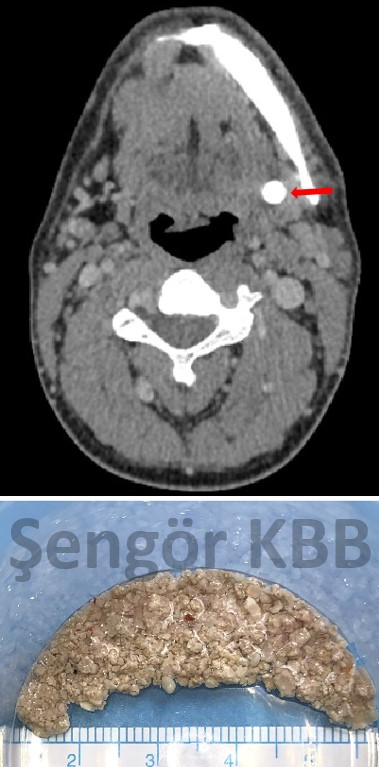
Tomografi Sonrası Kırılmış Tükürük Bezi taşı
Is every salivary gland swelling a stone?
Salivary gland stones are the most common cause of salivary gland swelling. They cause swelling under the chin (submandibular) or in the cheek salivary glands (parotid). Stenosis, which I briefly mentioned above, is the second most common condition. A part of the duct (segmentary stenosis) or sometimes the whole duct (generalised stenosis) may be narrowed. Or there may be stenosis/closure even only at the mouth of the canal. Unfortunately, interventions made with intraoral incisions without a sialendoscope are the most common cause of this type of stenosis. Saliva cannot pass through the narrowed area and the gland swells.
Swelling can sometimes also be due to autoimmune diseases (Sjögren’s disease) or radioactive iodine treatment. Radiation sialadenitis occurs in patients who have received radioiodine treatment for thyroid cancer. Juvenile recurrent parotitis is a recurrent inflammation of the parotid gland in childhood. Actually, the secretory cells (parenchyma) are involved in these cases, but we may also encounter duct stenosis during the disease process. We can help these patients by widening the salivary gland ducts with sialendoscopy.
There are other duct diseases that swell the salivary glands. We also encounter secretion concentrations (mucus plugs), duct polyps and foreign bodies.
Swollen salivary glands are not only caused by duct obstruction. Everyone has heard of mumps, which is mostly seen in children. In mumps, the secretory cells of the cheek (parotid) salivary gland become inflamed and swollen with the mumps virus. There may also be some masses in the gland that appear as swelling and gradually grow. These can be benign or malignant tumours. Sialendoscopic procedures have no place in mumps and tumours.
The common symptom of all these conditions is salivary gland swelling. In these diseases, we assess the duration of symptoms and examination findings. For example, in patients with salivary gland stones or duct stenosis, swelling is typically associated with meals.
Salivation is stimulated by eating, even by sour flavours or simply by smell. If there is an obstruction in the salivary duct, the secretion cannot drain and the gland swells. If the obstruction is not complete, the swelling gradually subsides. However, if the stone grows over time, the obstruction in the duct increases and it takes longer for the gland to descend. When the duct is completely blocked, the gland may remain swollen permanently.
Depending on the clinic, we determine preliminary diagnoses with some tests and imaging methods.
Is Sialendoscopy a New Technique? Is it available in every hospital?
We can no longer call sialendoscopy a new technique. It was first started to be applied in the world in the 1990s. In 2007, we developed the pneumatic stone crushing method in the canal. In 2008, we wrote the first book on this subject in our country. We introduced our crushing method to the world in Geneva at the 1st International Sialendoscopy Congress in 2012. We have progressed a lot since then; the Germans have also started to adopt this method in stone crushing (2019).
Therefore, we have been working on this topic in our country for 20 years as of 2024, the year we are organising this page. Since then, we have been trying to popularise this method among colleagues. We write articles and share posts so that patients also know, demand and benefit from it.
Unfortunately, the devices and tools used for sialendoscopy are not available in most hospitals. These tools are very sensitive and costly; in addition, sialendoscopy method requires advanced endoscopic experience. These two issues prevent sialendoscopy from becoming widespread in our country from the very beginning. Those who start the technique cannot finance it when their tools break down; unfortunately, they cannot continue.
Fortunately, we can now provide education in our country; at least we are not dependent on foreign countries. With our medical studies, I can say that we have been able to announce this issue to most of the ENT specialists in our country. Moreover, I am happy to see that this method has started to be applied in a few centres.
However, sialendoscopy tools are still not available in most hospitals, and the fact that they are available does not mean that they can be used by every specialist. The sialendoscopist must have adapted the stone crushing devices to the method in the hospitals where they perform the application.
In our practice, we use intra-canal crushing method and combined methods in cases with stones. This has enabled us to increase the success rate from 40% to over 90%.
Are any incisions made during sialendoscopy?
In sialendoscopy, we do not make an incision under normal conditions. We gradually widen the mouth of the salivary gland duct with thin rods called ‘dilators’. Then we advance the sialendoscope into the duct. With the intra-canal stone crushing method, we break the stones into small pieces. We remove the pieces from the canal by washing or holding them with fine tools. Under ordinary conditions, we complete the intervention without making any incision.
However, there may be cases where an incision is required with sialendoscopy. For example, the mouth of the salivary duct may be very narrow and resist expansion. In this case, we can make a 1-2 millimetre controlled incision called papillotomy. In this way, the mouth of the duct is opened and we can advance the sialendoscope. This incision may also be necessary for salivary gland stones that are stuck near the mouth of the duct. A proper papillotomy performed meticulously in this way prevents the duct from sticking in the future.
Sometimes there may be stones that are very difficult or impossible to remove sialendoscopically alone. An incision can be made on such stones that are found under the tongue or in the cheek. This incision, which can be called sialolithotomy or sialodocotomy, is called ‘salivary gland stone surgery’. Duct incisions made in the absence of sialendoscopy may result in failure or destruction of the duct. This can lead to adhesion, stenosis or even closure of the duct. In this case, the patient may also lose the chance of future treatment with sialendoscopy. Even if one stone is removed, other stones may remain behind.
If it is not possible to remove the stone in any other way, if an intraoral incision is absolutely necessary, great care should be taken. In this case, we first locate the stone in the canal with a sialendoscope. We make the incision exactly over the salivary gland stone. This meticulous procedure is called ‘sialendoscopy-guided approach through the mouth’. After removing the salivary gland stone, we re-enter the salivary gland duct with the sialendoscope. In this way, we check whether there is another stone left behind. If there are any remaining stones or dense salivary plugs, these are also removed by sialendoscopy. At the end of the intervention, we repair the duct with ductoplasty (sialodocoplasty) and insert a stent.

One Piece Salivary Gland Stone
Can large stones be removed with sialendoscopy?
We apply crushing method together with sialendoscopy. Since I have gained experience in this combination, the size of the stones only affects the working time. In this way, we can break and remove very large stones. We can break salivary gland stones with pneumatic lithotripsy (air pressure) or Holmium laser method. It may take 3-4 hours to break and remove large stones. In cases that will take a long time, I do not prefer laser in order not to damage the canal due to heat. I definitely and generally use pneumatic lithotripsy for large stones.
We need to see the salivary gland stone during sialendoscopy. We touch the stone crushing probe to the stone and break it with pneumatic shots. Some or parts of the stones may be buried; they may not be accessible. Therefore, it is useful to remind the success rates as follows. 80-85% of the stones can be reached by sialendoscope. Our success rate for the stones reached is 94% at the end of 20 years. These general rates are the same for small stones and large stones.
Is hospitalisation necessary after sialendoscopy?
Sialendoscopy is not a serious surgical procedure; it is an endoscopic procedure. During sialendoscopy, we perform a very meticulous and technical work inside the duct of the salivary gland. Therefore, the patient can be discharged on the same day after sialendoscopy.
We usually perform sialendoscopy under anaesthesia. This requires a hospital environment and the effects of anaesthesia may last for several hours. It is sufficient for the patient to rest for 5 hours after waking up in order to remove the anaesthesia from the body. Patients with prolonged anaesthesia may spend the night in the hospital. We have many patients coming from out of town or abroad. We keep some of them only for accommodation and discharge them the next day.
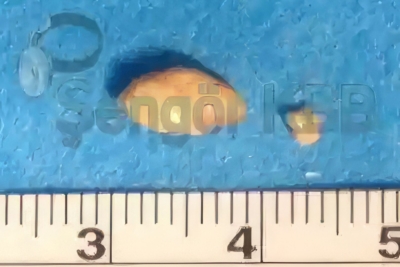
Large and Small Salivary Gland Stones
What is the treatment process after sialendoscopy?
During sialendoscopy, we work by giving fluid into the duct. After the operation, there is usually an additional swelling in the patient’s gland. This may last for a few hours or a few days. There is always a stent in the duct; this may slow down the flow of saliva a little. We remove the stent after 1 week on average; this is not a troublesome process. The patient drinking plenty of fluids and massage often helps the swelling to go down.
There may be mild pain due to swelling and stretching for the first 1-2 hours. In this case, paracetamol type painkillers are sufficient.
In cases where we remove the stone by sialendoscopy, the healing process starts immediately in the gland. After the stent is removed, swelling with meals also disappears. In time, the intensity and taste of the secretion also improves.
However, in cases where the problem has been present for years, it may take time for the gland to return to normal. Although the general hardness of the gland is largely improved, it may take months before it is like the healthy side. Rarely it is not the same; some swelling may remain. However, this situation should not be confused with salivary gland sagging due to aging.
Since it is an application performed through the mouth, it is necessary to take precautions against inflammation. For this purpose, we give antibiotics for 5 days during and after the operation for protection.
In some rare cases, it may be necessary to keep the stent in the canal for 2-3 weeks. We remove this thin plastic tube, which we fix to the oral mucosa with a silk, as easily as if we were removing stitches. This procedure, which we perform in the office, does not cause any discomfort to the patient.
How are the controls after sialendoscopy?
After sialendoscopy, we check the patients at certain intervals. We remove the stent at the end of 1 week on average. It is good to see that the canal works well and the consistency of the secretion at the end of the 2nd week and 1st month. We try to adapt these in patients coming from outside Istanbul.
There may also be cases that could not be treated with sialendoscopy and the stone could not be reached. This situation is 15-20 per cent. There may also be cases where some of the stones are left behind. In these cases, it is necessary to follow the swelling attacks and inflammation of the gland for a long time. Since we widen the duct during sialendoscopy, some of the stones can move in the duct with the flow of saliva. Some of them may fall out spontaneously within months or years. Sometimes, salivary gland stones may approach to a distance suitable for surgery. In these patients, a second sialendoscopic procedure may be useful. However, if the symptoms worsen and there is no tolerance, surgical removal of the gland may also be considered.
How long does it take to return to daily life after sialendoscopy?
Sialendoscopy is not a tiring procedure for the patient. If we have performed diagnostic sialendoscopy and used local anaesthesia, the patient can return to normal life on the same day. However, the procedure to crush salivary gland stones under general anaesthesia may take a long time. In this case, the patient should rest for 1-2 days.
Do private insurances cover sialendoscopy?
The policy contracts of private insurers are between them and their patients/customers. The insurers attach importance to the time of onset of the disease and the policy date. Under favourable conditions, most private health insurances cover sialendoscopic approaches.
Whether the insurance will approve the operation can be learnt after the application by filling out the policy form. According to the Turkish Medical Association and HUV scoring systems, sialendoscopy is 300 units. Sialendoscopic stone removal is 500 units. If sialodocoplasty (plastic repair of the salivary gland duct) is required, 300/2 units are added. If a minor salivary gland biopsy is required, 300/2 units will be added. The scope of the policy (how much of the agreed fee will be covered) should always be clarified by the patient’s insurance agent.