Reviews of those who have been treated for salivary gland stones vary depending on the operation and its outcome. There are basically three treatment methods. In the absence of sialendoscopy, salivary gland stones are removed through incisions made in the mouth. If this is not possible, surgical removal of the gland is even recommended. If the patient’s problem is solved, if the disease is cured, even if he/she has lost the gland, his/her comments may be positive. However, with sialendoscopy, we do not remove the gland but the stone; we even preserve the duct of the gland. This last method is not new anymore; I have been performing it in our country since 2004, but it is the most suitable for today’s ‘minimally invasive’ concept. Because today there are organ-sparing treatments that do not require salivary gland surgery to remove the stone.
The following are various cases of salivary gland stone removal and crushing, selected from the more than a thousand sialendoscopy operations I have performed to date. I have tried to select different cases depending on the size of the stone, its location, the length of time it was removed or crushed, and the difficulty of the operation.
1.Example Case

Parotis Bezi Taşı
This patient had swelling in his cheek for 1 month. He first consulted a dentist in case it was tooth-related. It was determined that there was an obstruction in the salivary gland (parotid gland) on the left cheek. Parotid gland stone was suspected and she was referred to me for sialendoscopic treatment. Ultrasonography revealed a 7.3 mm long, thin parotid gland stone. The day we agreed to remove the stone arrived. When I entered with a sialendoscope, at a distance of 3.5 cm from the duct mouth, the salivary gland duct was almost as narrow as a pinhead (pinhole stenosis).
It was a very resistant stenosis; I first widened this stenosis at the expense of bending the instruments, because I had to pass my 1.6 mm diameter sialendoscope through this area to remove the stone. This stage alone took 1.5 hours. Finally, I passed through the stenosis and reached the parotid gland stone, which was relatively easy to remove. Since the stone was soft, it was breaking even with forceps (grasping tool). But until the last stage, it was not clear whether the case would be successful or not. I was almost ashamed of the patient and my colleague from Trakya University who had come to watch. I checked the end/fine branches in the gland; all stone fragments had been removed. I made an additional application so that the canal stenosis that I had widened would not close again. I placed a stent in the canal to be removed after 1 week.
It is not possible to know such conditions in advance; we can only see them during sialendoscopy. Therefore, sialendoscopy should first be considered as a diagnostic method. After seeing the inside of the canal, stone, stenosis, etc., we start working. It is not possible and correct to talk about success without seeing it. I can give certain rates to patients; for example, the probability of reaching a stone with sialendoscopy is 80-85%. However, it is not possible to remove such a stone without sialendoscopy. Untouchable parotid gland stones and stenosis in the duct do not allow any other intervention.
Without sialendoscopy, this patient could only be offered a parotidectomy to remove the gland. Fortunately, with sialendoscopy, experience, complete equipment and effort, we can often overcome such situations. We are very glad that we were able to save this patient from #parotidectomy surgery.
2. Example Case

Salivary gland stone one piece
This patient is a 31-year-old male patient. For 15 days he had swelling under the right jaw. Considering the length of the stone, a 5 millimetre stone grows in about 5 years. It is interesting that he had no symptoms before. It may have recently progressed in the canal and got stuck in the narrowest exit section. The swelling must therefore have just started. The salivary gland stone you see in the picture was stuck 0.5 cm from the duct opening/outlet. During the operation, I made a small mucosal incision of a few millimetres after slightly widening the canal orifice. Then I removed the salivary gland stone by grasping it with a forceps.
I then entered the duct with a sialendoscope and found that the rest of the duct system was slightly dilated, and there were accumulated condensed secretions, which we call mucus plugs. I washed them out and checked the canal down to the fine branches to see if there were any more stones. I then reconstructed the mouth of the canal with repair work (sialodocoplasty). I do this so that the canal heals well, does not narrow, and any future deposits do not petrify and fall out. To ensure this, I inserted a thin plastic tube (stent) into the canal, which will remain in place for 7 to 10 days.
When should root canal incisions be performed?
Stones very close to the mouth of the duct and larger than 3 millimetres can also be removed with intraoral incisions. Salivary gland removal with a sialendoscope may not be possible at short distances. If it is forced, it may injure the canal entrance. If a duct incision is made, the duct must be repaired afterwards. Otherwise, the duct may narrow or close if the incision is left in place. Canal incisions are one of the methods we use together with sialendoscopy when necessary.
It should be emphasised that this should be performed under the guidance of sialendoscopy. In conditions without sialendoscopy, we see stones left behind. In such patients, swelling of the salivary gland may continue; their problems remain unresolved. The situation is also troublesome when the duct incision is made but not repaired. In these cases, if the duct narrows or adheres, the chance of treatment with sialendoscope becomes difficult. Especially if the duct is destroyed, sometimes it is not possible. One week later, I removed the stent because the secretion from the duct was very good and well healed. We removed the salivary gland stone, preserved the functioning of the duct and took precautions to prevent the stone from recurring.
3. Example Case
Salivary Gland Stones
Salivary gland stones with and without crushing
Many people are surprised to learn that stones can form in the salivary glands and cause problems. They have heard of kidney stones, gall bladder stones and dental stones before, but they wonder whether stones can also form in the salivary gland. Drinking less water, smoking and not eating enough vegetables facilitate the formation of stones in the salivary gland…
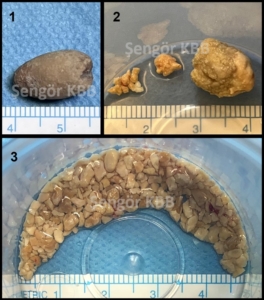
Image description:
In the first picture, a large parotid gland stone in the cheek was removed by an intraoral approach guided by sialendoscopy.
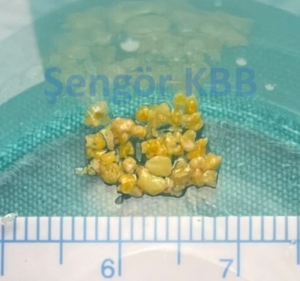
In the second picture, a large, near-surface stone in the root of the tongue was removed by incision. The other stones in the duct could only be accessed with a sialendoscope and one was removed by crushing.
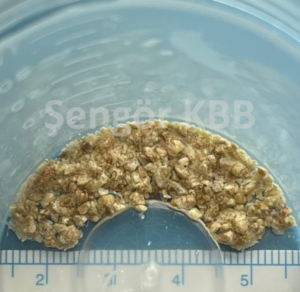
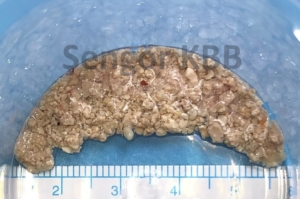
In the third picture, an intra-glandular stone of almost 3 centimetres, which was not palpable, could be removed by sialendoscopic lithotripsy. With the combination of sialendoscopy, pneumatic lithotripsy and intraoral surgery, I can say that the success rate in the removal of salivary gland stones has increased to 94% after 20 years.
4. Example Case
Our patient is a teacher from Izmir. The stone was embedded in the gland and was 15x13x12mm in size. There was a class L3b salivary gland stone that could not be felt during the examination.
The sialendoscopy was very difficult. From the first minute to the last moment, I was not sure if I could remove the entire stone. But I tried until the end and broke the huge stone by performing 1351 pneumatic blows in 4 hours. I completely cleaned the pieces from the canal.
Whether the stone is in the gland, in the canal, big or small does not matter in this level of sialendoscopic study. According to the results I have obtained from my studies, I can give some rates to my patients. 80-85% of the stones can be reached with sialendoscopy; my success rate in the stones reached is 94%.
5. Example Case

Submandibular salivary gland stone
This submandibular salivary gland stone belonged to a colleague working in Istanbul. The stone could not be seen in the ultrasonography performed due to the complaint of salivary gland swelling. However, the stone could be seen in the floor of the mouth during the examination in the office. When I entered the canal with the sialendoscope, I saw that the stone had moved into the gland. It was seated in the hilum (center of the gland) and was approximately 10×3 mm in size. I removed it from the canal that I had widened by holding it with forceps and pulling it.
It took about 45 minutes including anesthesia. Some stones cannot be detected with ultrasonography and tests. However, we can often diagnose these during the examination or during sialendoscopy. The Doctor’s stone was not small, but since it was thin, it had moved towards the gland in the canal. However, this situation helped me to remove the stone without breaking the canal.
Although this stone seemed easy at first, it could not have been removed without sialendoscopy because it had gone to the bottom. Although the doctor experiences additional stress in patients, when the result is successful, it is replaced by a similar level of happiness.
6. Example Case
Large submandibular salivary gland stone broken
This patient is from Ankara. Sialendoscopy had been attempted for submandibular salivary gland stones before, but it could not be performed because the canal could not be entered. The intraoral incision that was made thereupon was also unsuccessful. Since the stone was large, it was recommended that the entire gland be removed with open surgery. In his tomography, there was a huge stone measuring 17x12x12 mm in the gland. During the operation, I saw that the canal mouth had disappeared due to the incision made in the past. It was not possible to enter the canal from here, but a depression was observed in the projection of the gland at the level of the tongue root. This depression was the opening (fistula) area of a past infection. I was able to reach the salivary gland stone by widening it. I completely cleaned the stone by breaking it with sialendoscopy; I made 697 pneumatic shots and it took a total of 2.5 hours. I always get anxious during revision, or secondary cases. Moreover, this patient had so much faith and trust in me… In order to relieve some of the pressure on me, we talked in detail about the possibility that I might not succeed. Patients need to know all the possibilities regarding the sialendoscopy technique. I always talk about these with every patient. Although the success rate is 94%, when the 6% probability of failure occurs, this high rate is meaningless. Fortunately, I was able to successfully overcome this very difficult case.
7. Example Case
Broken Salivary Gland Stone
This patient’s salivary gland stone was also inside the gland. It was 4.5 cm from the canal mouth and 7 mm in diameter. I broke it into pieces with 142 shots using the pneumatic crushing method under sialendoscopy and removed it in 1.5 hours. The size of the stones does not prevent them from being removed with sialendoscopy; it only prolongs the operation time. Advanced endoscopic experience and a long learning period are essential for success in sialendoscopy. It also requires technology, money, passion and patience.
Click for detailed information about Salivary Gland Stone Treatment.
